An intrauterine device (IUD) left in a woman for more than 20 years may have contributed to a nasty infection that sent her to the emergency room, doctors in Japan reported this week. The long-expired birth control device was found surrounded by bacteria that caused her months of fever and abdominal pain. Once the woman had the IUD removed and she was given a long course of antibiotics, her symptoms cleared up.
IUDs are T-shaped devices, no bigger than a quarter, that are inserted into the uterus and used as long-term birth control. This usually happens through the release of hormones from the device or from the copper or other materials that some products are made with (the copper makes the uterus inhospitable to sperm). IUDs are 99% effective at preventing pregnancy, but like all medications, they have drawbacks. The initial insertion process can be very painful, for instance, while some people can experience symptoms like increased bleeding or cramps in the months after. They were also probably a lot less safe when they came out in the 1970s than they are now.
One other limitation, depending on how you look at it, is that they’re not meant to last forever. Different brands have different expiration dates, but all IUDs are supposed to be replaced or removed after some number of years. For a copper IUD, the one with the longest replacement time, users are still advised to take it out after 10 to 12 years. Unfortunately, the woman in this case study, published in the New England Journal of Medicine on Wednesday, didn’t do so.
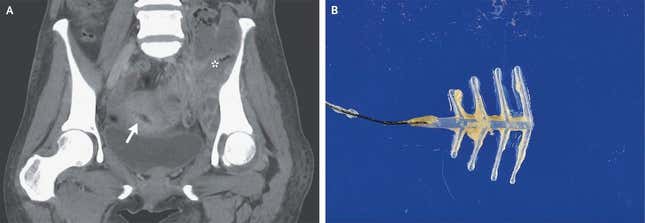
According to the report, the 54-year-old woman visited the ER after suffering symptoms for quite some time. She had been experiencing a fever and weight loss for two months, as well as abdominal pain and difficulty walking for three weeks. Upon examination, doctors noticed a tender mass on her lower left abdomen, while blood tests revealed an elevated white blood cell count, a common sign of infection. When the woman underwent a CT scan of the affected area, doctors spotted the IUD, along with multiple abscesses (pus-filled pockets of dead tissue, white blood cells, and germs that are a sign of infection) throughout the pelvis and extending out to her left hip joint. Doctors performed an operation to drain the abscesses and wash out the fluid in her hip to physically clear as much of the infection as they could. They removed the IUD at the same time.
The long embedded device was coated in distinctive “sulfur-colored” granules often associated with a group of rod-shaped bacteria known as actinomyces (the granules are ball-like masses of the bacteria clumped together with pus gunk). And sure enough, when they tested fluid samples from the woman, they were able to isolate the bacteria Actinomyces israelii. This kind of infection is known as actinomycosis.
Though A. israelii is a common and usually harmless passenger in the vagina, colon, and mouth, it can occasionally cause opportunistic infections. Study author Noriko Arakaki told Gizmodo in an email that the IUD probably did play a role in the woman’s ordeal, given that these infections have been linked to IUDs left inside for too long (not to mention, the device was covered in the bacteria). In this case, the woman’s IUD was a plastic, non-hormonal device that should have been replaced after five years at most, while annual check-ups are also recommended. Though the authors didn’t ask why the woman opted not to replace it as expected, Arakaki noted that she was not fond of hospitals.
“Pelvic actinomycosis occurs in more than 85% of cases where the IUD has been used for more than 3 years and is more common in users of plastic IUDs than copper IUDs,” Arakaki said. “We consider that the long-term use of IUDs is a factor in this case.”
The woman was subsequently treated with a prolonged course of IV antibiotics, followed by oral antibiotics. Though she is still taking oral antibiotics, she’s in “good general health with no recurrence of abscesses and no major complications,” Arakaki said.
The authors hope their study will remind other doctors to consider the possibility of actinomycosis in similar cases where pelvic abscesses are found, and to look into their patient’s IUD history as well. “Secondly, it is important that the patient understands that the IUD must be used properly, that regular outpatient visits are necessary, and that it must be replaced at the appropriate time,” she added.